Reports Overview
When assessing Breast Cancer, an accurate picture requires specific information on many different factors. Your medical reports combined give you a picture of the status of your breast cancer and suggests a path for standard of care treatment. Being willing to pivot in treatment, maybe several times, in order to identify the most effective strategy for your sub-type of breast cancer can be beneficial to identify effective treatment or maybe even crucial to your survival.
It is vital that you have an accurate understanding of all your test results before you can make good treatment decisions for yourself.
BCA is here to help you better understand your reports after your doctor has given you your test results.
Book a Consult with Roxann

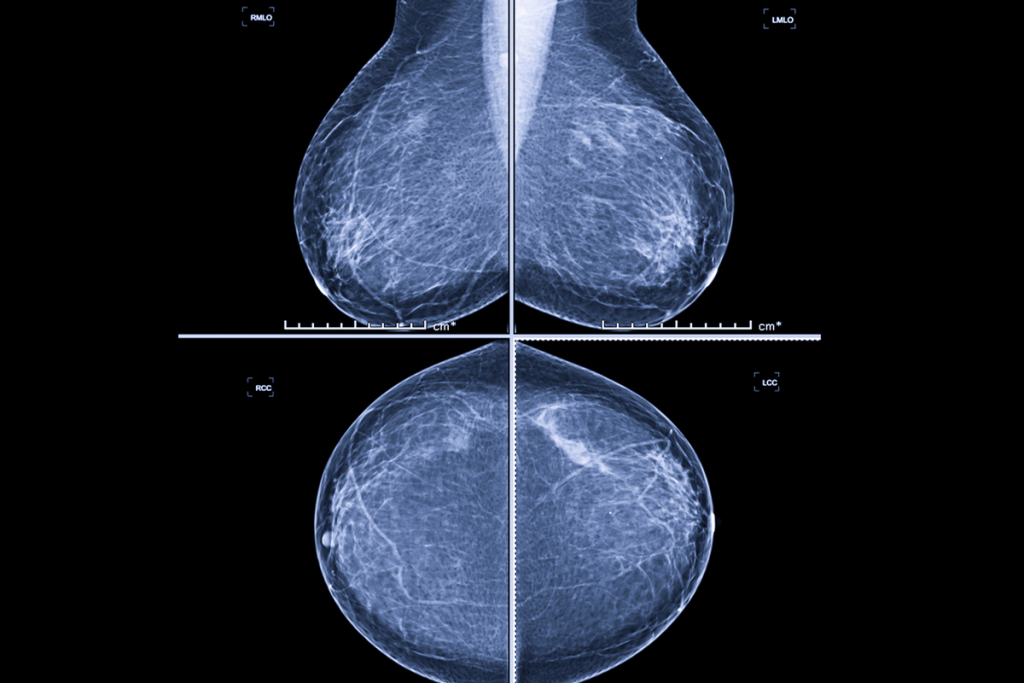
What is a Bi-Rads Score?
Your Mammogram and MRI reports will have a Bi-Rads score on them along with the Radiologist’s findings explaining that score – all in medical lingo. This score is a way to categorize the findings of the scan by the Radiologist. The score is based on the Radiologists’ interpretation of their findings of your likelihood of breast cancer from that scan. . Your ordering physician will go over your results with you and refer you to a breast surgeon if the Radiologist recommends it.
BI-RADS categories
- BI-RADS 0: Incomplete, additional imaging is needed Usually attached to Bi-rads 5
- BI-RADS 1: Negative, no significant abnormalities. Only found for women with no history of breast surgery
- BI-RADS 2: Benign, noncancerous growth, such as a cyst or fibroadenoma or women with a history of breast surgery with no suspicious findings because there is scar tissue present. This is the lowest rating for a woman with a history of any kind of breast surgery. Any breast surgery will have scaring and therefore some type of benign findings of abnormalities that are not concerning.
- BI-RADS 3: Probably benign, but a follow-up study is recommended
Also for women with a history of breast surgery with no suspicious findings – because there is scar tissue that looks different than normal breast tissue - BI-RADS 4: Suspicious, may be cancerous, and requires a biopsy 2%-95% cancer – a very big unhelpful category. That may require a repeat MRI or biopsies depending on the Specialist Doctor’s opinion. Most Breast Oncologist Surgeons and Medical Breast Oncologists read their own Breast MRI’s
- BI-RADS 5: Highly suggestive of malignancy, requires a biopsy.
Most likely breast cancer. This was Roxann’s original MRI finding on her right breast. - BI-RADS 6: Known biopsy-proven malignancy, requires treatment.
This was Roxann’s finding on her left breast after biopsy
These reports can be frustrating to read, especially at Bi-Rads 4 because to a certain extent these are only educated guesses based on an opinion, although educated, and is only a suggestive direction for your doctor. And, if you have been diagnosed with cancer prior and this is a re-staging or treatment surveillance MRI or you are waiting to know if you are diagnosed with breast cancer the waiting is an off the chart anxiety attack for days to a week while you are waiting for the results of your pathology.
Pathology Reports
These reports contain a wealth of information about the breast cancer a woman has – and are very complicated to read when you don’t understand the terms and what they mean for you.
We suggest you get yours out, if you have it, make a copy of it –and then be ready to mark it up with a pen so you will remember later what you learned here now.
What Information does My Pathology Report Contain & Why is it Important?
This is your first report and identifies what Type of Breast Cancer you are diagnosed with.
For One-on-One Help With Your Reports Subscribe Below

Choose Your Membership
Unlock Exclusive Content, Expert Guidance, and Premium Features by Selecting the Membership Plan That Best Suits Your Needs. Join Today – Take The First Step Toward YOUR Healing!
Already a member? Log in here