Standard of Care Treatments
The current Standard of Care (SOC) for breast cancer in the US was developed in the 1980s & 90s. It is the combination of surgery, chemotherapy, radiation, and hormone therapy began to crystallize as the gold standard in breast cancer treatment in the U.S.
The unfortunate truth is that this basic treatment model has not changed much in 40 years!
The “chemotherapy” category of standard treatment has been broadened to include immunotherapy and more toxic drugs that are not actually chemo but are included in this category of treatment because they are given to treat cancer.
The “gold standard of breast cancer treatment” is adjusted or the sequence of treatment is re-ordered based on the type and stage of the breast cancer, per a standard protocol for that – and despite what doctors may lead patients to believe, this “gold standard” lacks true personalization for individual women at any stage of breast cancer. Ultimately, Standard of Care treatment involves the same limited toxic treatment protocols for all women, with the main variations being when chemotherapy is used and what other specific toxic drugs are prescribed.

Surgery: Early Stage (0-II) Breast Cancer
Lumpectomy
A lumpectomy, also known as breast-conserving surgery or partial mastectomy, is a surgical procedure to remove a tumor or other abnormal tissue from the breast while preserving most of the breast. During the procedure, the surgeon removes the cancerous tissue along with a small margin of healthy tissue around it.
When is it done?
Lumpectomy is typically performed to treat early-stage breast cancer, stages 0-2.The goal is to remove the cancer while maintaining the appearance and shape of the breast.
How is it done?
An incision in the breast to remove the tumor and a small rim of normal tissue around it. The surgeon then closes the incision, and the breast is reshaped if necessary. In some cases, a lumpectomy may be performed along with a sentinel lymph node biopsy to check if the cancer has spread to nearby lymph nodes.
Complications
As with any surgery, lumpectomy carries some risks, including:
- Infection at the incision site
- Bleeding or hematoma formation
- Swelling or bruising
- Pain or discomfort
- Changes in breast appearance or sensation
- Lymphedema is swelling in arm/hand/trunk due to lymph node removal during Mastectomy
Success Rates
Stage 0 – 1 Lumpectomy
With Radiation:
- 5-year survival rate: Approximately 99%.
- 10-year survival rate: Around 90%.
Without Radiation:
- 5-year survival rate: Approximately 90%.
- 10-year survival rate: Around 80%.
Stage 2 Lumpectomy
With Radiation:
- 5-year survival rate: Approximately 99%.
- 10-year survival rate: Around 90%3.
Without Radiation:
- 5-year survival rate: Approximately 90%.
- 10-year survival rate: Around 80%
Lumpectomy is often followed by Radiation Treatment.

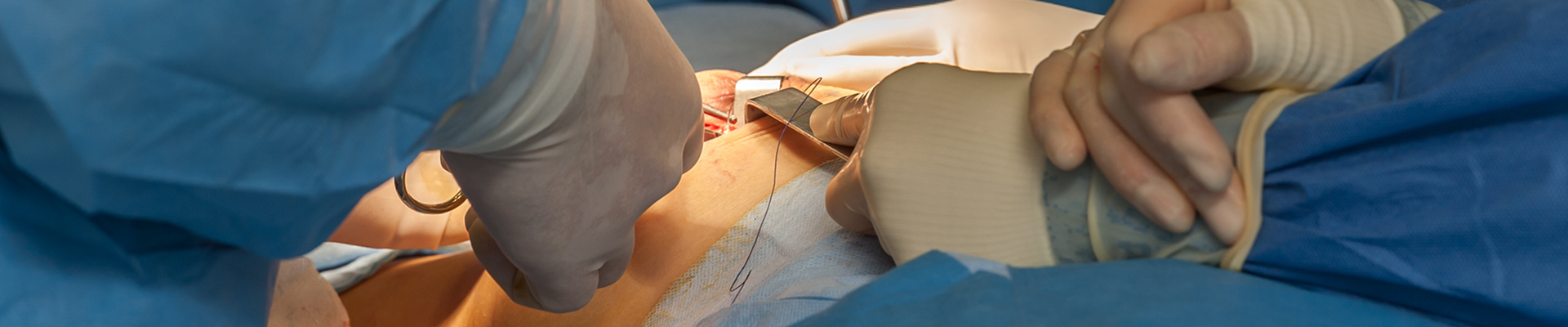
Surgery: Later Stage (II-IV) Breast Cancer
Later stage breast cancer surgery is a Mastectomy. There are several types and your surgeon will recommend the type that will best your type and stage of breast cancer.What is a Mastectomy?
A mastectomy is a surgical procedure to remove all or part of a breast. It’s most commonly performed to treat or prevent breast cancer.
Mastectomy is the surgical removal of a breast, an amputation. It is performed to treat diagnosed breast cancer or as a preventative measure for high-risk individuals. Women with cancer in both breasts will have a bilateral mastectomy, the amputation of both breasts, as can women who have cancer in one breast to avoid a future diagnosis and treatments in the healthy breast.
Breast tissue extends well beyond the area covered by bra cups. It spans a large region from the sternum to the armpit, down to the ribs, and vertically from the collarbone to the ribcage. Understanding this helps to grasp the significant amount of tissue removed during a mastectomy.
A Mastectomy has significant psychological consequences for a woman and she requires substantial emotional support after undergoing a Mastectomy to regain a healthy emotional balance and to be able to create a new perspective for her life
Different Types of Mastectomy
There are several types of mastectomy, each varying in the amount of tissue removed:- Simple (Total) Mastectomy: Removes the entire breast, including the nipple, areola, and skin.
- Modified Radical Mastectomy: Removes the entire breast along with the lymph nodes under the arm.
- Radical Mastectomy: Removes the entire breast, lymph nodes, and chest muscles under the breast. This is less common today3.
- Skin-Sparing Mastectomy: Removes breast tissue, nipple, and areola but preserves most of the breast skin.
- Nipple-Sparing Mastectomy: Similar to skin-sparing but leaves the nipple and areola intact. When this type of surgery is chosen an additional surgery is needed to preserve the Nipple Areola Complex (NAC).
Why is it done?
A mastectomy is done to treat breast cancer or as a preventative surgery to reduce the risk of developing it, especially in individuals with a high genetic risk (e.g., BRCA1 or BRCA2 gene mutations).
What is Nipple Delay Surgery?
Nipple delay surgery is a preparatory procedure performed before a nipple-sparing mastectomy (NSM). It aims to improve the blood supply to the nipple and surrounding skin, reducing the risk of complications like tissue necrosis (death) during the subsequent mastectomy.Why is it done?
Nipple delay surgery is done to enhance the chances of preserving the nipple-areolar complex (NAC) during a mastectomy, especially in patients with a higher risk of complications due to factors like large breast size, previous radiation, or drooping breasts.
How is it done?
- Incision: The surgeon makes an incision around the nipple and releases the undersurface of the nipple and surrounding skin from the breast.
- Blood Supply Improvement: This allows the blood vessels in the skin under and around the nipple to dilate, improving blood flow.
- Waiting Period: The patient waits for about two weeks to allow the nipple to adapt to the new circulation pattern before the Mastectomy is done.
Complications of Mastectomy
Approximately 20-33% of women experience some form of complication after a Mastectomy. Because Mastectomy is much more extensive surgery than Lumpectomy there are many and more serious complications.
The emotional and psychological impacts of Mastectomy are real and should be addressed. Good emotional support both from other breast cancer survivors and family and friends are essential for a woman to have a good quality of life after receiving a breast cancer diagnosis and while going through treatment and beyond. A breast cancer diagnosis, no matter the stage, is traumatizing.
The most common include:
- Wound infection: Redness, swelling, warmth, and discharge from the breast.
- Seroma: Fluid buildup causing swelling and discomfort, often needing drainage.
- Hematoma: Blood collection causing pain and swelling, sometimes requiring drainage.
- Shoulder stiffness: Pain and limited movement. This complication can be avoided by doing the mastectomy exercises given to you by your doctor.
- Lymphedema:
Mastectomy Success Rate
The following statistics are general and individual patient outcomes will vary based on the Type of Breast Cancer the Stage of Breast Cancer, her general overall health and her age. Your Breast Cancer Doctors will give you their medical opinion about your expected outcome. Mastectomy is always followed by Radiation treatment in breast cancer patients.
Mastectomy With Radiation
- 5-year survival rate is about 86%.
- 10-year survival rate is around 70%.
Mastectomy Without radiation
- 5-year survival rate is about 75%,
- 10-year survival rate is around 60%.
BCA questions why, if standard of care treatment is so successful why are 25% of women dying in 5 years and another 30-40% for a total of 65% of women dying from breast cancer in 10 years of diagnosis?

Radiation Therapy
When is Radiation Treatment Advised?
Radiation therapy is typically recommended after surgery (like a lumpectomy or mastectomy) to eliminate any remaining cancer cells and reduce the risk of recurrence. It can also be used to alleviate symptoms in advanced cases where cancer has spread to other parts of the body. There are several types of Radiation Therapy available for Breast Cancer Patients. Your Medical Oncologist typically decides which type is best for a specific patient in conjunction with the Breast Oncologist Surgeon.
Traditional Radiation
How is it Done?
There are two main types of radiation therapy for breast cancer:
- External Beam Radiation Therapy (Traditional Radiation): This is the most common type. A machine called a linear accelerator delivers high-energy beams of radiation to the affected area. The patient lies on a table, and the machine moves around them to target the cancer from different angles.
- Brachytherapy (Internal Radiation): After surgery, a radiation-delivery device is temporarily placed in the breast. Radioactive sources are placed in the device for short periods over the course of treatment.
Number of Treatments
The number of treatments can vary, but typically, Radiation is given to breast cancer patients 5 days a week for 6 weeks for a total of 30 treatments. Brachytherapy usually involves fewer sessions, often completed in a week.
Side Effects
Short-term side effects include:
- Skin changes (redness, irritation, peeling)
- Fatigue
- Breast swelling and tenderness
- Breast pain
- Lymphedema (swelling in the arm or hand) (interlink to this page)
Long-term side effects include:
- Changes in breast appearance (size, shape, texture)
- Lymphedema (persistent swelling) interlink again
- Heart and lung problems (because the radiation field includes these areas)
- Secondary cancers
Traditional Radiation Therapy has significant side effects – both short and long term. It’s important to discuss all potential side effects with your healthcare provider to understand what to expect and how those can be managed – and if this treatment is right for you.
Proton Radiation for Breast Cancer Patients
Proton radiation therapy is a type of radiation treatment that uses protons (positively charged particles) to target and destroy cancer cells. Here’s a detailed overview.
When is it Recommended?
Proton therapy is recommended for breast cancer patients because the cancer is located near critical organs such as the heart and lungs because they are right behind the left breast – the most common breast to develop breast cancer. It’s particularly beneficial for patients who have had previous radiation therapy in the same area or those at higher risk of complications from traditional radiation therapy.
How is it Different ThanTraditional Radiation?
Proton therapy involves directing a beam of protons specifically at the tumor. Unlike traditional radiation therapy, which uses X-rays (photons) that pass through the tumor and continue through the body, proton therapy stops at the tumor – the beam does not hit the vital organs(heart & lung) beyond the breast or chest wall tumor. This precision minimizes damage to surrounding healthy tissues and organs.
Number of Treatments
The number of treatments can vary, but proton therapy typically involves daily sessions over several weeks, similar to traditional radiation therapy an mirrors Traditional Radiation in that breast cancer patients typically have 30 sessions.
Possible Side Effects
Short-term side effects may include:
- Skin irritation and redness
- Fatigue
- Breast swelling and tenderness
- Nausea
Long-term side effects can include:
- Changes in breast appearance (size, shape, texture)
- Lymphedema (persistent swelling) – less likely since the beam is specifically directed
- Heart and lung problems (unlikely since the beam stops at the tumor site)
- Secondary cancers (rare)
Benefits Over Traditional Radiation
Proton therapy offers several advantages over traditional radiation therapy, especially for breast cancer patients:
- Precision: Proton therapy delivers radiation directly to the tumor with minimal exposure to surrounding healthy tissues. This significantly reduces the risk of damage to critical organs like the heart and lungs.
- Reduced Side Effects: Due to its precision, proton therapy is associated with many fewer side effects and complications than Traditional Radiation Therapy.
- Targeted Treatment: Proton therapy is particularly beneficial for tumors located close to vital organs as is the case with Breast Cancer patients or in women who have been previously irradiated and have a recurrence.

Lymphedema
Lymphedema is a complication of both Breast Cancer Surgery and Radiation Therapy. It can happen after one or both of these treatments in the short term or years later.
It is a blockage in the lymph system due to lymph node removal during mastectomy that causes welling and discomfort in the arm, hand and sometimes the trunk. This is a life long complication that is very debilitating, time consuming – and quite frankly, ugly.
This complication can be largely avoided as a Mastectomy complication by receiving a well-established very low risk preventive surgical solution with a 70-90% success rate. This surgical treatment can also be performed if Lymphedema develops after Radiation Treatment.
Lymphedema Bypass Surgery that can be performed during your mastectomy surgery performed by a microsurgeon ( a plastic surgeon with additional training) who can also perform your tissue expander or direct implant surgery.
Note Roxann was not offered the option of Lymphedema Bypass (LVB) surgery by either her breast or plastic surgeon when discussing her bilateral mastectomy with lymph node removal with them, which led to her developing lymphedema. When she eventually learned about LVB, she underwent this (additional) surgery, which completely cured her lymphedema. She is angry that it wasn’t offered to her as a preventative measure at the time of her mastectomy. LVB surgery completely cured Roxann’s lymphedema. She highly recommends this excellent procedure as a preventative at Mastectomy. Ask your surgeon about it when planning your Mastectomy surgery.
Hyperthermia
What is Hyperthermia?
Hyperthermia is a medical treatment that involves heating body tissue to high temperatures (up to 113°F or 45°C) to damage and kill cancer cells. It’s often used in combination with other cancer treatments like radiation therapy and chemotherapy to enhance their effectiveness. The heat makes cancer cells more sensitive to these treatments, potentially improving outcomes.
When is Hyperthermia Recommended?
Hyperthermia is typically recommended for treating advanced cancers that haven’t responded well to other treatments. It’s used for cancers such as breast, cervical, esophageal, liver, lung, melanoma, and sarcoma and has been available for more than a decade.
Benefits of Hyperthermia
- Enhanced Effectiveness: When combined with radiation therapy and chemotherapy, hyperthermia can make these treatments more effective by making cancer cells more sensitive to heat.
- Targeted Treatment: Hyperthermia can target specific areas, minimizing damage to surrounding healthy tissues.
- Alternative for Surgery: It can be an option for patients who aren’t healthy enough for surgery or for tumors that are difficult to reach surgically.
Side Effects of Hyperthermia
Short-term Side Effects
- Pain: The treatment area may become painful.
- Swelling: Some swelling may occur at the treatment site.
- Burns: There’s a risk of burns if the heat isn’t controlled properly.
Long-term Side Effects
- Tissue Damage: Prolonged exposure to high temperatures can cause damage to healthy tissues.
- Infection: There’s a risk of infection at the treatment site.
Insurance Coverage
Hyperthermia treatment is not widely available and is still under investigation in clinical trials. Medicare covers Hyperthermia when administered in conjunction with Radiation Therapy. As such most coverage by insurance has expanded greatly so it is usually covered in 2025. It’s best, however, to check with your insurance company to verify your coverage before undergoing treatment. Most medical facilities will do this for you before beginning a course of treatment.

Chemotherapy
When is Chemotherapy Recommended for Breast Cancer Patients?
Chemotherapy is recommended in several situations:
- Adjuvant Chemotherapy: After surgery to eliminate any remaining cancer cells and reduce the risk of recurrence.
- Neoadjuvant Chemotherapy: Before surgery to shrink tumors, making them easier to remove.
- Metastatic Breast Cancer: When cancer has spread to other parts of the body and surgery isn’t an option.
When is Intravenous (IV) Chemotherapy Recommended?
IV chemotherapy is administered through a catheter placed in a vein, usually in the forearm or hand. The drugs can be given in different ways:
- IV Push: Drugs are injected quickly through the catheter using a syringe.
- IV Infusion: Drugs flow from a bag through tubing attached to the catheter, controlled by an IV pump.
- Continuous Infusion: Infusions can last from 1 to several days, controlled by electronic IV pumps.
Number of Doses for Breast Cancer Patients
The typical number of chemotherapy doses is a course of treatment includes 4 to 8 cycles, with each cycle lasting 2 to 6 weeks. Each cycle includes multiple treatment sessions followed by a break to allow the body to recover. Individual treatment cycles may vary.
IV Chemo Side Effects
Short-term side effects include:
- Nausea and vomiting
- Fatigue
- Hair loss
- Increased risk of infections
- Mouth sores
Long-term side effects include:
- Heart damage
- Lung damage
- Nerve damage
- Secondary cancers
- Infertility – if you are of childbearing age it is critical that you discuss your fertility with your doctors before beginning Chemotherapy to plan for your future.
Success Rate of IV Chemotherapy for Breast Cancer Patients
The success rates of chemotherapy for breast cancer varies depending on the stage and type of breast cancer, as well as individual factors such other health conditions and age.
Chemotherapy can be incredibly taxing on the body. Many cancer patients evaluate their prognosis and the expected quality of life during and after chemotherapy before deciding to pursue this treatment option because Late Stage Breast cancer survival rates are low 30- 60%.
Chemotherapy in Pill Form for Breast Cancer
Types of Drugs:
- Capecitabine (Xeloda): Commonly used for metastatic and advanced stage breast cancer.
- Cyclophosphamide (Cytoxan): Can be taken orally, though more commonly given via IV.
- Vinorelbine (Navelbine): Used in Europe for breast cancer, though not approved in the U.S.
- Methotrexate: Used in combination with other drugs for early and advanced stages.
Dosing:
- Dosage varies based on the specific drug, cancer stage, and patient’s health. It’s crucial to follow the doctor’s instructions precisely.
Length of Treatment:
- Typically, treatment spans 3-6 months, administered in cycles with rest periods in between to allow the body to recover.
Benefits:
- Convenience: Can be taken at home, reducing hospital visits.
- Less Pain: Avoids the discomfort of IV infusions.
- Immune System Safety less exposure to COVID-19 and other infections: Reduces exposure to hospital environments.
- Geographic Convenience: Beneficial for those in rural areas.
Short-Term Side Effects:
- Nausea and Vomiting
- Fatigue
- Hair Loss
- Loss of Appetite
- Diarrhea or Constipation
Long-Term Side Effects:
- Bone Marrow Suppression
- Heart Damage
- Secondary Cancers
- Neuropathy (nerve damage)
Success Rate:
The success rate varies depending on the type and stage of breast cancer, but many oral chemotherapy drugs have shown similar effectiveness to traditional IV chemotherapy. Even “ at-home” chemotherapy places a significant strain on the body, and as a result, many breast cancer patients carefully consider this option as well. This deliberation is especially crucial when facing late-stage breast cancer, where survival rates are low ranging between 30% and 60%.

Hormone (Suppressing) Therapy
What is Hormone Therapy?
Hormone therapy, also known as endocrine therapy, is a treatment for hormone receptor-positive breast cancers. These cancers rely on hormones like estrogen and progesterone to grow.
Medications Available
There are several types of hormone therapy medications available:
- Selective Estrogen Receptor Modulators (SERMs):
- Tamoxifen: Commonly used for both premenopausal and postmenopausal women. It’s taken daily in pill form.
- Toremifene: Similar to tamoxifen, used for advanced breast cancer in postmenopausal women.
- Aromatase Inhibitors (AIs):
- Anastrozole (Arimidex): Used for postmenopausal women.
- Letrozole (Femara): Also for postmenopausal women.
- Exemestane (Aromasin): Used after initial treatment with other AIs.
- Estrogen Receptor Down Regulators (SERDs):
- Fulvestrant (Faslodex): Used for advanced breast cancer.
- Ovarian Suppression:
- Goserelin (Zoladex): Used in premenopausal women to suppress ovarian function.
- Leuprolide (Lupron): Another option for ovarian suppression.
Dosing
The dosing for these medications varies:
- Tamoxifen: Typically taken as a 20 mg tablet daily for 5-10 years.
- Aromatase Inhibitors: Usually taken once daily, with specific dosages depending on the medication (e.g., 1 mg of anastrozole, 2.5 mg of letrozole, 25 mg of exemestane) for 5-10 years.
- Fulvestrant: Administered as an injection, with a loading dose followed by maintenance doses for as long as it remains effective.
- Ovarian Suppression: Administered via injection, with dosing schedules depending on the specific medication for as long as it remains effective.
Side Effects
Short-term Side Effects:
- Hot flashes
- Night sweats
- Vaginal dryness
- Mood swings
- Fatigue
Long-term Side Effects:
- Increased risk of blood clots (especially with tamoxifen)
- Bone thinning and osteoporosis
- Increased risk of endometrial cancer (tamoxifen)
- Joint pain and stiffness
Success Rates
Hormone therapy has been shown to significantly reduce the risk of breast cancer recurrence & survival rates in the short-term. Studies have demonstrated that taking tamoxifen for 5 years can lower the chance of breast cancer recurrence by about 40%. Aromatase inhibitors have also been effective in reducing recurrence and improving outcomes in postmenopausal women but only in the short term.

What is Immunotherapy?
Immunotherapy is a type of cancer treatment that helps your immune system fight cancer. It works by either stimulating your immune system to work harder or by providing it with components like man-made immune system proteins.
Immunotherapy is recommended for triple-negative breast cancer (TNBC) and high-risk early-stage breast cancer. It’s also used for metastatic breast cancer that has spread to other parts of the body.
How is it administered to breast cancer patients?
Immunotherapy for breast cancer is typically administered through intravenous (IV) infusion. This method involves delivering the immunotherapy drug directly into a vein, usually in a hospital or outpatient clinic setting. The infusion is typically given every 2-3 weeks, depending on the specific drug and treatment plan.
Dosing
The duration of immunotherapy infusions for breast cancer patients can vary widely based on several factors, including the type of immunotherapy, the stage of cancer, and how well the patient is responding to treatment. Some patients may experience significant benefits and continue treatment for an extended period, while others may stop earlier due to side effects or lack of response. It’s important to work closely with your healthcare team to determine the optimal duration for your specific situation.
Short-term side effects can include:
- Fatigue
- Nausea
- Skin rash
- Diarrhea
- Cough
- Poor appetite
Long-term side effects
- serious autoimmune reactions, where the immune system attacks healthy tissues, potentially affecting the lungs, liver, intestines, and kidneys.
Success Rate
The success rate of immunotherapy varies, but drugs like pembrolizumab (Keytruda) have shown improved survival rates in patients with high PD-L1 expression. Clinical trials continue to evaluate its effectiveness, with some showing durable responses in patients.
Based on the seriousness of these side effects patients often consider prognosis an quality of life before deciding on this treatment.
Insurance Coverage
Insurance coverage for immunotherapy can depend on the specific plan and the type of immunotherapy used. It’s best to check with your insurance provider to understand the coverage details and any out-of-pocket costs.
- Off Label
- Alternative
- Combination

Empower Yourself Now!
More Resources
Emotional Support is critical to your healing. Even if everything goes smoothly with your treatment a cancer diagnosis is stressful. Reach out to your support network to help you emotionally on a regular basis. A Therapist is a very good idea.
And then use Duality to fill in the gaps!
References
- National Comprehensive Cancer Network (NCCN) – Provides Standard of Care breast cancer treatments
- World Health Organization (WHO) – Discusses Standard of Care breast cancer treatments
- PubMed – National Library of Medicine – Reviews Standard of Care breast cancer treatments.
- National Cancer Institute (NCI) – Covers standard treatments
- Centers for Disease Control and Prevention (CDC) – Provides a general overview of breast cancer treatments
- American Cancer Society (ACS) – Discusses local and systemic treatments